
Causes
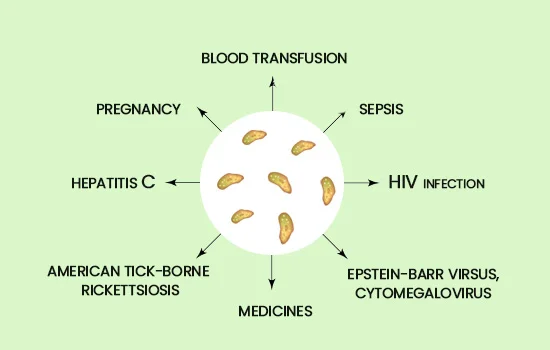
The exact cause of ITP is still unknown and various studies are underway to attempt to understand why our bodies might react this way. It is not curable, but with proper treatment can typically be managed. Studies have shown some things that are known to trigger ITP:
-
Viral infections like chickenpox, HIV or Epstein Barr virus.
-
Luekemia or lymphoma
-
Rheumatoid arthritis or Lupus
-
Some medications including chemotherapy drugs
-
Pregnancy
Symptoms
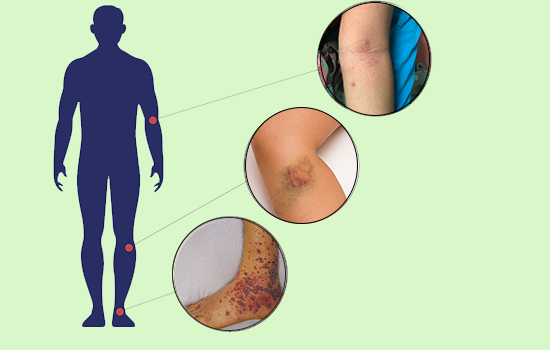
There are several typical visible symptoms that signal a person may be experiencing ITP.
-
Easy Bruising: Bruises can appear without any known trauma.
-
Purpura: Bleeding under the skin, similar to bruises, but can be spread over a larger area of the body.
-
Petechia: Tiny red dots appear in the skin.
-
Bleeding: Gums bleeding when brushing teeth, nose bleeds, heavy menstrual periods, blood in the urine or stool.
Diagnosis
ITP diagnosis starts with a complete blood count (CBC) test to check the number of platelets in the blood. Urine and stool samples may also be collected to check for the presence of blood.
A serious possible symptom of ITP is a brain bleed. This symptom can be life threatening and is not visible like the other symptoms. Patients must be very careful not to incur any trauma to the head during a bout of ITP. In rare cases, a brain bleed during ITP can occur even without any trauma to the head.


Treatment
Treatment depends on the age of the patient, their overall health condition, and previous medical history. The doctor will look into the patients’ reactions to certain medicines and immunity. Close monitoring of platelet counts and preventing any external injury or bleeding is key.
For children, the body may recover on its own; in some cases in as few as 2 to 4 days. Adults may require continued treatment.
The most common initial treatment is steroids. Steroids slow down platelet destruction but come with some side effects such as irritability and weight gain.
If steroids don’t work, the typical next treatment is intravenous immune globulin (IVIG). Immune globulins come from the blood of donors. They contain antibodies that bind to the cells of the spleen preventing it from killing the platelets. IVIG also comes with some side effects such as headaches, nausea, fever and chills.
Doctors will sometimes supplement or alternate IVIG treatments with an IV infusion of Rituximab (Rituxan). Rituxan is a monoclonal antibody that is produced in a lab. It is used in the treatment of cancers such as non-Hodgkin lymphoma. It slows down antibody production, which in turn slows down the destruction of platelets. There are some side effects with Rituxan including chest pain, chills, confusion and cough.
In chronic cases, doctors will sometimes recommend splenectomy. This is because the spleen is what is killing the platelets. Removing it can sometimes eliminate the problem. This procedure comes with surgical risks such as blood clots and infection. Additionally, living without a spleen increases likelihood of infections, some of which can be serious or life-threatening. For this reason, your doctor may recommend you take vaccines, and use preventive antibiotics.
In some more severe cases, when platelet counts don’t increase after the above things have been tried, doctors may consider the use of NPlate (romiplostim). NPlate is a prescription medicine designed to attach to special cells in the bone marrow, increasing platelet production. It is administered via weekly injection under the skin. Before each injection your doctor will draw blood to confirm your platelet count. It, too, comes with some side effects including blood clots, weakness and nausea.
In the most extreme cases, such as a catastrophic hemorrhage requiring an invasive surgical procedure, where life-threatening bleeding may occur, doctors may recommend one or more platelet transfusions. These transfusions include platelets from one to four carefully screened blood donors. These platelets are given via drip into the vein for about 30 minutes, and so this procedure is sometimes called a platelet infusion. Infusing these platelets into the blood stream can sometimes raise the patient’s platelet count. This procedure also has some side effects including shivering and skin rash.
To help prevent recurrence, your doctor might focus on changing any medications that could have triggered your ITP, or if an infection could be the culprit, may focus on ensuring you have completely healed from it.
Managing ITP
Though ITP may not be cured; it can sometimes be controlled so that the patient can lead a somewhat normal life. An important part of the treatment is regular follow ups. It is recommend that you keep a detailed history of all tests and check-ups as it helps the physician to understand the progress and draft any changes if required.
It is also important to avoid injuries during an ITP bout. Avoid playing sports, especially those that could result in impact to the body or head. At extremely low platelet levels, it is even considered dangerous to go up or down steps, as a simple fall could be very dangerous. That said, it is still recommended to remain active, doing things like taking walks.
It is also recommended that you pay attention to over-the-counter medications and supplements as some have the potential to lower platelets or have anti-clotting effects.
As you begin to navigate life with ITP you may find a support group helpful. A great one for ITP is the Platelet Disorder Support Association (PDSA). They have lots of stories of people dealing with ITP as well as a page on vitamins and other supplements that may be helpful in the treatment of ITP. They also fund research and education.